Hartsdale Keratoconus and Specialty Contact Lens Center
Hartsdale Keratoconus and Specialty Contact Lens Center
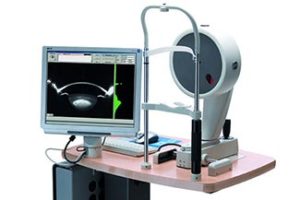
We use state-of-the-art technology including corneal topography and external digital ocular photography to diagnose & identify patients with corneal diseases like keratoconus. We have an extensive inventory of diagnostic contact lenses and professional resources allowing Dr. Arlene Schwartz to prescribe the best solution for your visual needs.
Our center can successfully manage keratoconus without surgery in many cases. We also fit specialty gas permeable, scleral lenses and specialty soft contact lenses to manage patients with severe dry eyes, corneal scarring, irregular astigmatism and corneal transplants. We have many patients who visit us from the surrounding areas of Scarsdale, Ardsley, White Plains because of our expertise with hard to fit contact lenses.
Detection for Keratoconus & Other Eye Disease
We use a slit lamp, advanced digital imaging, and Pentacam topography to identify and manage progression of corneal eye disease or conditions that would require a specialty contact lens solution.
Plus, Dr. Schwartz’s years of experience alone helps her to identify patients with subtle cases that could go undetected.
Our Specialty Services
We provide specialty eye care services for individuals who have eye issues and chronic eye diseases that cannot be corrected by traditional eyeglasses and contact lenses. Our optometrist, Dr. Arlene Schwartz, has witnessed first-hand hundreds of patients that have experienced the life-changing effects of our specialties.
Dr. Schwartz has extensive relationships with other optometrists, ophthalmologists, corneal specialists, and general care doctors that refer specialty patients because they know they can count on her professional knowledge and patient care.
What Kind of Contact Lenses Can Help Someone With Keratoconus?
Scleral Contact Lenses for Keratoconus
Scleral lenses are typically the size of a nickel to a quarter. These specialty lenses rest on the white part of the eye, or sclera, and trap a fluid cushion between the cornea and contact lens, providing a smooth, artificial front surface to bend light. While scleral lenses have existed for a while, only more recent technological advances have made these designs available in clinics that routinely manage irregular corneal conditions such as keratoconus.
Not only do scleral contact lenses vault the cornea, but the design fits the sclera far better. There are specialty toric-designed scleral lenses that match the curve of the cornea and sclera. This means that we have various materials and coatings for these lenses to provide greater comfort & wetness for dry eye patients and sensitive eyes.
Besides treating keratoconus, scleral lenses can also provide a healthy, comfortable lens-wearing experience for patients experiencing extreme dry eye or post-LASIK ectasia.
Because of proficiency and belief in the effectiveness of scleral lenses, we are currently using the three main brands for scleral lenses:
- AmpleEye
- Acculens
- Zen lens
- Boston sight lens
Other Specialty Contact Lens Options for Keratoconus
Custom Soft Contact Lenses
These Novakone & Kerasoft lenses are thicker soft contact lens designs that are able to offer comfort and clear vision in many cases when regular soft contact lenses are not able to successfully correct the high degree of astigmatism associated with keratoconus and other corneal eye diseases.
Rigid gas permeable (GP)
RGP contact lenses are most commonly prescribed. If eyeglasses or soft contact lenses cannot control keratoconus, then gas permeable (GP) contact lenses are usually the preferred treatment They provide a smooth, artificial surface to mask the “peaks and valleys” of the keratoconic cornea, in turn providing the best vision. The keratoconus center at Hartsdale Family Eyecare uses a variety of lens designs, and the best contact lens for you will be determined following a complete evaluation. But GP contact lenses can be less comfortable to wear than soft lenses. Also, fitting contact lenses on a keratoconic cornea is challenging and time-consuming. You can expect frequent return visits to fine-tune the fit and the prescription, especially if the keratoconus continues to progress.
Soft contact lenses can used in combination with GP contact lenses, often referred as piggybacking to improve comfort.
Hybrid contact lenses
Hybrid contact lenses have a relatively new design that combines a highly oxygen-permeable rigid center with a soft peripheral “skirt.” Manufacturers of these lenses claim hybrid contacts provide the crisp optics of a GP lens and wearing comfort that rivals that of soft contact lenses. Hybrid lenses are also available in a wide variety of parameters to provide a fit that conforms well to the irregular shape of a keratoconic eye.
What Causes Keratoconus?
 Often beginning in teens, keratoconus usually progresses into the 20s or 30s before stabilizing, although in severe cases it can continue to worsen. In these cases, the cornea continues to thin and bulge outward, creating even greater blurred vision. Scarring of the cornea can spontaneously develop.
Often beginning in teens, keratoconus usually progresses into the 20s or 30s before stabilizing, although in severe cases it can continue to worsen. In these cases, the cornea continues to thin and bulge outward, creating even greater blurred vision. Scarring of the cornea can spontaneously develop.
More than 1 in 1,800 people have keratoconus, according to researchers. In ten percent of cases, patients report a family member who has keratoconus, Risk factors for oxidative damage and weakening of the cornea include a genetic predisposition, explaining why keratoconus may affect more than one member of the same family but keratoconus has no race or gender correlation.
Research suggests the weakening of the corneal tissue that leads to keratoconus may be due to an imbalance of enzymes within the cornea. This imbalance makes the cornea more susceptible to oxidative damage from compounds called free radicals, causing it to weaken and bulge forward.
Keratoconus is also associated with overexposure to ultraviolet rays from the sun, excessive eye rubbing, a history of poorly fit contact lenses and chronic eye irritation.
Many keratoconus patients also suffer from hayfever, eczema and asthma. Some researchers feel that eye rubbing may increase the progression of keratoconus. Although it hasn’t been proven that eye rubbing exacerbates keratoconus, it is still a good idea to refrain from rubbing your eyes. Dr. Schwartz may prescribe eye drops to minimize eye itching symptoms.
Commonly Asked Questions About Keratoconus
Keratoconus & Surgical Treatments
Dr. Schwartz works closely with ophthalmologists who perform corneal crosslinking and identify keratoconus early to slow the progression of this eye disease.
Specialty contact lenses are the first-line treatment of choice for keratoconus, but for some patients, surgery may be needed. A small number of keratoconus patients get corneal transplants, but this is the last resort.
Corneal Collagen Cross-linking
C3-R (corneal collagen cross-linking with riboflavin): This FDA approved procedure, is a non-invasive procedure that involves placing eye drops containing riboflavin (vitamin B2) on the cornea, which are then activated by ultraviolet (UV) light to strengthen links between the connective tissue (collagen) fibers within the cornea. It’s recommended to young, keratoconus patients in their teens or early 20s because it helps slow the progression of the disease.
Intacs
An alternative to transplants is Intacs® prescription inserts, also known as intrastromal corneal ring segment implantation. Intacs are generally an option when a wearer cannot tolerate GP lenses, but the keratoconus has not progressed to the point of needing a transplant. Glasses or contacts may still be needed after such a procedure; but soft contact lenses might provide acceptable vision in these circumstances, Scleral lens design is also an option when other lens choices do not offer an acceptable vision.
Several studies show that Intacs can improve the best spectacle-corrected visual acuity (BSCVA) of a keratoconic eye by an average of two lines on a standard eye chart. The implants also have the advantage of being removable and exchangeable. The surgical procedure takes only about 10 minutes. Intacs might delay but can’t prevent a corneal transplant if keratoconus continues to progress.
Corneal transplant:
Some people with keratoconus can’t tolerate a rigid contact lens, or they reach the point where contact lenses or other therapies no longer provide acceptable vision. The last remedy to be considered may be a cornea transplant, also called a penetrating keratoplasty (PK or PKP). Even after a successful cornea transplant, most keratoconic patients still need glasses or contact lenses for clear vision.
